23 June 2022 (updated: 23 June 2022)
Telemedicine Benefits and Challenges to Know Before Building Your Own Telehealth App
Chapters

Telehealth possesses an enormous potential to reinvent healthcare systems worldwide. See the challenges to address & benefits of building your telehealth app.
Introduction
COVID-19 changed the world. It cost lives; it revealed shortcomings in our healthcare system; it set groups against each other over social responsibility vs personal freedoms; and it caused geopolitical strife, worldwide.
Essential lockdowns to contain the pandemic made accessing healthcare much more difficult. However, it also gave rise to new, remote solutions. Nowadays, telemedicine benefits are being delivered through telehealth apps faster and more efficiently than ever before.
In this article, we’re going to discuss some of the top barriers to telemedicine and how they are being overcome to reach patients online. We’ll also shed light on the benefits accessing healthcare via telehealth apps has brought into the world.
What are the main telehealth challenges?
Here are some of the top telehealth challenges, as identified by the Board on Health Care Services; Institute of Medicine, Washington:
User experience
Your software engineering team will be challenged to create a functional and usable UI/UX. One part of the app will be for patients and will have a strong visual element for the face-to-face aspect. However, it should also take into consideration language, age, and ability to enter data before the appointment. This may include magnifying portions of the screen for vision-impaired, audio for the blind, and visual cues and captioning for the deaf. It should suit tablets and phones as well.
The other part is for the medical professional. This will have different functionality based on analytical needs. The physician may ask for data such as pulse, O2 saturation, and blood pressure, if the patient has it available, and will need a place to enter it. The ability to highlight such data on the UI will aid them in assessing or diagnosing the patient. They will also need the ability to keep notes, create prescriptions, and send those to the correct pharmacy.
Reimbursement
Now that many large payers are ready to get onboard, telehealth apps must offer patients secure credit card payment options, or a billing tool to identify insurers. For service providers, it should identify the CPT/HCPCS codes and 95/GT modifiers during the billing process.
Telehealth apps trigger assorted legalities depending on jurisdiction. Telehealth challenges include several states that won’t recognize a doctor from a neighboring state, or allow an out-of-state patient. Medicare limits where it is applicable (rural, institutional, specific CPT codes, etc.) While a nationally recognized license for medical professionals is in the works, it doesn’t yet exist so the app must be aware of limitations on payment and reimbursement.
 Source: Unsplash
Source: Unsplash
Security and telehealth challenges
Hacker attacks increase every year because of hospitals’ administrative inertia. Stunningly, there are hospitals “saving money” by still running on antique and no-longer-supported operating systems like WINDOWS XP, 98, or even 95! Why? They still use other older software that is dependent on those ancient operating systems that would be costly to replace.
The foregoing is a systemic problem outside of your responsibility. While telehealth apps can be vulnerable because they handle highly-sensitive data—your answer is through simple risk mitigation. Once data reaches your app, it cannot “leak” anywhere on its journey from patient to provider. As a telehealth app developer, your responsibility is to encrypt all data transmissions and storage.
The main weakness is when data is sent outside of your control. It is important that data archiving on devices (physician’s computer/patients’ devices) should be equally inaccessible outside of the system. You may not be able to prevent someone from stealing your app files from a hospital, but you can assure that it is a string of useless encrypted digits and letters that are of no use to them.
Wearable devices sending data by cellular, Wi-Fi, or Bluetooth are essentially invulnerable when using 128-bit or 256-bit encryption (aka bank-level encryption). The industry needs to enhance data protection on (or replace) older wearable medical devices, but you need to do it now, before your telehealth app enters the market. There may be other points of failure, but your clients need to have confidence in your product—that their personal, private data is protected.
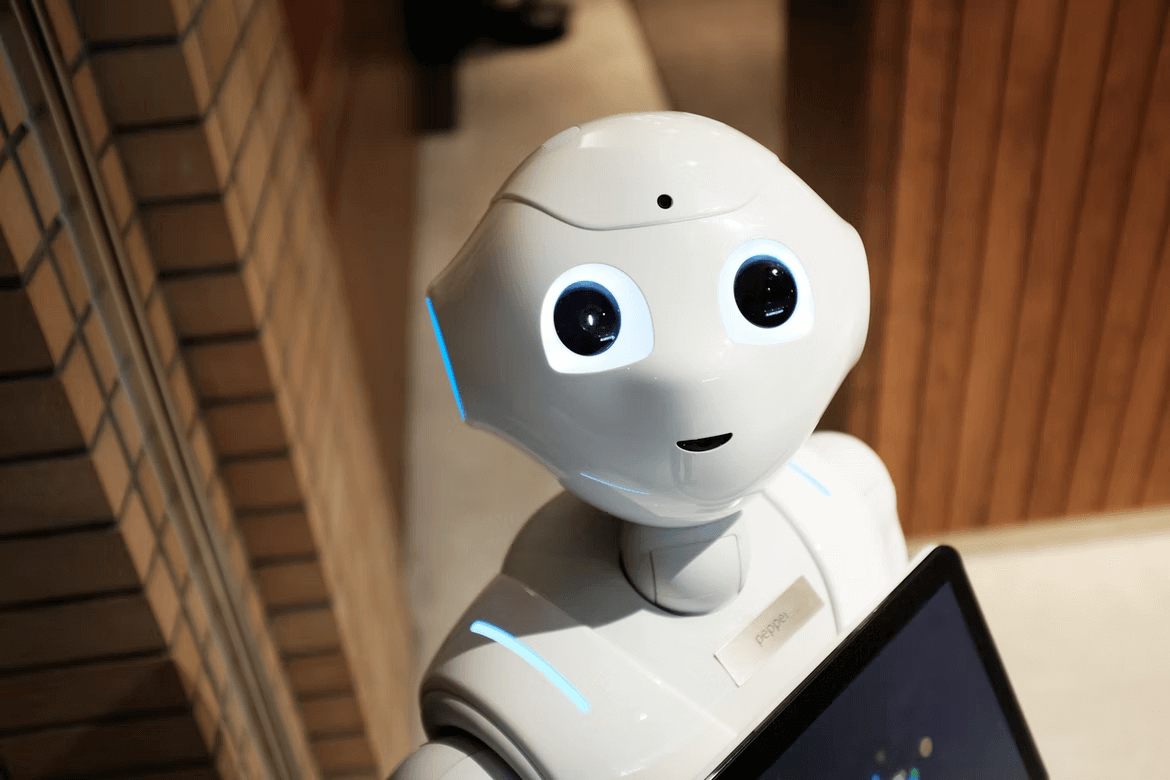
Technology & data interoperability
The technology selected for your telehealth app determines how it integrates with other software. See more on interoperability in healthcare. Whether used by hospitals, institutions, doctors, or health app users, it is important to choose the right language, data management, encryption technology, and a useful framework for the app.
 Source: Unsplash
Source: Unsplash
Limited evidence to support success
Arguably, we’ve been enjoying telemedicine benefits since 500 B.C.E., when Greek doctors would consult with patients by messenger, treating many while never leaving their homes. Modern communications have lowered the barriers to telemedicine from hours to seconds.
Modern telehealth is a new area, which is still being explored. The lack of evidence may lie in the chosen methodology to prove its effectiveness. Specifically, one attempted study was to look at congestive heart failure treatment by telemedicine, but they couldn’t get people to sign up because patients feared being in the “control group” and not getting proper treatment.
The solution was more obvious—treat all volunteer patients to achieve telemedicine benefits, note the success rate vs. standard in-person care, and then note the cost savings. This provides persuasive numbers for the large payers.
Conversely, some applications of telemedicine show great progress; they may still require some synthesis of existing studies to evaluate their dollar value. Some large payers are ready to implement telemedicine, but await such evidence in regard to cost savings.
Four reasons to create a telehealth app
Patients demand telehealth apps
The financial benefits and additional flexibility for healthcare services are the impetus to invest in this market. Patients and providers are beginning to accept these programs since a large part of our population is mobile, living in one state and sometimes working in another.
The notion of denying them coverage because they are “out of network” is completely inappropriate, especially during an emergency. Telehealth apps can connect them to telemedicine benefits they’re entitled to, effectively eliminating complicated claims and paperwork.
Additionally, telehealth allows access to consults with specialists that may not be available locally. Eliminating excessive travel while sick is invaluable to many.
Patients obtaining those benefits continue to grow annually worldwide. In the U.S. nearly 10 million patients utilized telemedicine (some without even knowing it because of consults behind the scenes) in 2021, up from 7 million in 2018. While that is just 3% of the population, the trend is growing.
Since telehealth services are available 24 hours per day, and seven days per week it is easy to see why three-quarters of U.S. consumers would be open to using telemedicine services. The same proportion would forego live human interactions in favor of access to medical services on demand.
Companies dedicate budgets to telehalth specifically
While more than half (56%) of healthcare executives say they have already implemented telemedicine in their organization, some organizations are considerably further along than others. About 24% are currently investigating preliminary telemedicine options, while the remainder are just learning about it for the first time.
Pandemic caused a change in habits
Altered behavior due to the COVID-19 pandemic was the first reason to consider investing in developing a telemedicine app. It drove telemedicine use up immediately at the start of the pandemic (100x or 10,000%) among both patients, and medical professionals, but has now settled down to a steady slow growth from 3,800%. Eliminating these barriers to telemedicine is manifesting as a quarter trillion dollar industry by 2025 that is set to grow even bigger.
Recently, Statista showed that about 70% of U.S. citizens are open to using a telemedicine app upon need. Those users who are fully satisfied with their experience with telemedicine services also topped 70%. They fully expect to utilize telehealth services again when required. Wait times are short (generally under 20 minutes); fees are low (average $40); and, most importantly, telemedicine allows them to get on with their lives.
The technology may not be completely routine yet, but it is gaining broad acceptance. There is always room for your new product, particularly if it is well-designed and suits both physicians and patients, while considering the needs of insurers.
A promising landscape for securing funding
The market capitalization for telemedicine should reach $194 billion by 2023, a quarter trillion by 2025, and likely $460 billion by 2030. While initially driven by the pandemic, cost-saving for both consumers and insurers, overall convenience, practicality, and the sheer speed and availability of service will drive the development forward.
 Source: Statista
Source: Statista
Summary
Medical telehealth is inevitable now that so many have seen it in action, acknowledge its effectiveness, and appreciate its convenience, plus modest cost. It also provides multiple benefits to doctors, who can save time on paperwork and consulting minor health issues such as colds, all the while not sacrificing the quality of care.
Now is the time to begin your research and development. There is still space for you in this growing market, but make sure to do an exceptional job and create an app that is bug-free, considers all users’ needs, and won’t be supplanted by someone who took a little more care in the design than you did.
Check out also
- How to design & develop a healthcare app? — The ultimate challenge for modern healthcare is to create scalable apps that solve the right problems while looking sleek.